[ad_1]
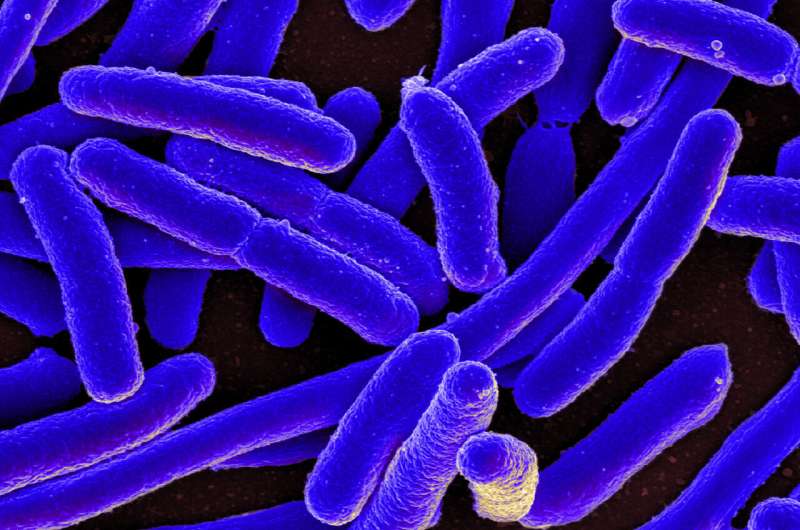
A new study led by researchers at University of Utah Health details a novel mechanism that infectious bacteria use to quickly adjust to environmental stress. The discovery could help explain why certain types of common infections—such as urinary tract and bloodstream infections like sepsis—are hard to get rid of.
The mechanism, described in the journal Nucleic Acids Research, alters the precision with which the bacteria make proteins, complex molecules that carry out most of the work in cells. These changes may improve the bacteria’s chance for survival.
“Understanding how pathogens survive stressful situations can reveal new targets for development of anti-microbial drugs and vaccines,” said Matthew Mulvey, Ph.D., professor of pathology at U of U Health.
Adapt or die
When bacteria infect their host, they are exposed to stress, such as extremely salty or acidic environments or novel antibiotics, that could easily spell doom for the pathogen. If the stressor cripples even one of the key pathways that the bacteria need to survive, the entire population could die off.
However, bacteria can adapt, an ability that relies on a slight twist to basic principles of biology.
Dogma says that each gene contains instructions for making a single kind of protein. A molecule called transfer RNA (tRNA) then uses these instructions to oversee the production of proteins. In times of stress, though, random changes to the tNRA-mediated process can be an especially quick way to alter a cell’s array of proteins. This can generate useful new proteins that help the organism to thrive.
“There is a growing appreciation that a little bit of noise in the system can be good,” Mulvey said.
Shifting expectations
The discovery came from a bit of serendipity. A former graduate student in Mulvey’s lab stumbled upon a bacterial enzyme called MiaA that turned out to be both particularly sensitive to environmental stress and central to the regulation of protein expression. In one experiment, he created a version of an especially pathogenic bacteria that lacked the gene that encodes MiaA.
“Every kind of stress we exposed the MiaA-deficient strain to seemed to cause problems,” said the study’s co-first author Matthew Blango, Ph.D, who is now a junior research group leader at the Leibniz Institute for Natural Product Research and Infection Biology in Jena, Germany. “So, we really thought that this protein might be playing an important role in gene regulation.”
Bacteria without MiaA did not grow well and did not cause urinary tract infections or sepsis in mice. This also occurred when the researchers manipulated the bacteria into expressing too much MiaA. “There appears to be a Goldilocks zone, where just the right amount of MiaA allows the optimal stress response,” Blango said.
Seeing how badly things went when MiaA levels were out of balance, former graduate student Brittany Fleming, Ph.D., the study’s co-first author, investigated further. She discovered that knocking out MiaA caused random “frameshifting”—an error where tRNA delivers three-letter genetic codes to be translated into proteins that are off by one letter. For example, a genetic code of “cat cat gta” might read as “atc atg ta…” when frameshifted. In the bacteria, the result of such a shift was impaired production of important proteins and production of unexpected proteins.
Additional experiments by co-first author and graduate student Alexis Rousek showed that changing levels of MiaA could alter the availability of key metabolites that feed into other important stress response pathways within the bacteria. These findings implicate MiaA as a key player within a web of pathways that can impact pathogen stress resistance.
Mulvey says his lab’s next step is learning how environmental stress alters MiaA levels within bacteria.
The implications for this research may extend beyond infection control. Humans express a version of MiaA that is linked to certain cancers and metabolic diseases. “What we learned about how MiaA works is likely to be relevant to research on cancer and other non-infectious human diseases,” Mulvey said.
Brittany A Fleming et al, A tRNA modifying enzyme as a tunable regulatory nexus for bacterial stress responses and virulence, Nucleic Acids Research (2022). DOI: 10.1093/nar/gkac116
Citation:
Study provides clues on why some bad infections persist (2022, March 23)
retrieved 23 March 2022
from https://phys.org/news/2022-03-clues-bad-infections-persist.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
[ad_2]
Source link





